Injury management
Injuries are a part of any contact sport. Serious or life threatening injury in Rugby is, however, rare. The outcome of many injuries can often be improved by very simple first aid skills until emergency help arrives. For the majority of the Rugby-playing world, there is little qualified medical support available pitch side. Thus, first aid responsibility may fall to club officials, coaches, players, parents, or referees.
Often when faced with an injury, the issue is what not to do rather than what to do, i.e., ‘do no further harm’. Many things improve with a little bit of time and, commonly, taking control of a situation and preventing panic is all that is needed until the player improves or more experienced help arrives. In certain circumstances, simple measures such as protecting the head and neck, ensuring an open airway or supporting an injured limb are often all that is needed in the immediate stages of injury management.
There are, of course, some conditions where the idea of simply supporting the player and waiting will be the wrong thing to do, e.g. cardiac arrest. These, while rare, do occur and are one reason for ensuring there is trained first aid support available at games and training.
World Rugby recommends that there is an appropriate level of first aid cover at every game and training session. World Rugby provides different levels of training and more details can be found at https://passport.world.rugby/player-welfare/first-aid-in-rugby/
The general principles of looking after an injured player are:
- Do no further harm
- Take control
- Avoid unnecessary movement
- Speak to the player
- Call for help if needed
- Ensure more experienced help is on the way
- Recognise when you need to do more which may include calling an ambulance

Take control of the situation.
Preventing panic until the player improves or more experienced help arrives is fundamental to looking after an injured player.
First Aid in Rugby
https://passport.world.rugby/player-welfare/first-aid-in-rugby/
All stakeholders - coaches, referees, parents, and anyone else involved in the Game - should undertake at least basic first aid training
For non-life-threatening and non-limb-threatening injuries
Assess the player on the field of play using the TOTAPS system.
| Steps | Assessment | Action |
| Talk | What happened? Where does it hurt? | |
| Observe | Look at the injured area. Is it different from the other side (swollen, a different colour, etc.)? | If swollen or there is a deformity, call first aider. |
| Touch | Feel for swelling, tenderness and pain. | If tender to touch, call first aider. |
| Active movement | Ask the player to move the injured part without assistance. | If unable to move or painful to move, call first aider, and remove from the field (non weight-bearing). |
| Passive movement | If the player moves the injured part actively, then carefully move it through a full range of movement. | If unable to do so or painful, the player should be removed from the field (non weight-bearing). |
| Skill test | If the active and passive movements did not produce pain, ask the player to stand and see if lower limb is fully weight-bearing and he/she can walk. If unable to do so, the player should be removed from the field (non weight-bearing for lower limb injuries). | If unable to do so, the player should be removed from the field (non weight-bearing). |
Bleeding
When treating a bleeding player, gloves should be worn to protect the player and the first-aider from possible transmission of blood-borne diseases such as HIV and hepatitis. Blood must not be transferred from one player to another. Any items that have been contaminated by blood must be sealed in a plastic bag and discarded appropriately.
 Major bleeding must be treated as soon as possible to reduce the flow of blood, as this may be enough to preserve a life. Apply direct pressure to a wound first and only apply indirect pressure if this is not possible. Arrange urgent transport to a hospital or doctor’s surgery.
Major bleeding must be treated as soon as possible to reduce the flow of blood, as this may be enough to preserve a life. Apply direct pressure to a wound first and only apply indirect pressure if this is not possible. Arrange urgent transport to a hospital or doctor’s surgery.
Soft tissue injuries
Soft tissue injuries are typically ligament sprains and muscle strains, tears and bruises. They should be treated using the method known as PRICED.
| Protect | Once an injury has occurred, it is of vital importance that the injured area and the player are protected from further injury. Failure to do so can exacerbate the problem and delay healing.
|
| Rest | Adequate rest to enable tissue healing and repair is vital for any injury. Remember - if it hurts, it is probably not good for the injury. Don’t put any weight on the injured part of the body. |
| Ice | Application of ice to an injury helps prevent bleeding and further swelling. Regular use of crushed ice in a damp towel is helpful in shortening recovery time and decreasing pain in the interim. Apply ice to the injury for 20 minutes every 2 hours for the first 48 hours. Protection of the skin with petroleum jelly or oil avoids unnecessary thermal injury. |
| Compression | Compression of a soft tissue injury prevents swelling and shortens recovery time. Compression using a firm bandage is effective. Ensure that bandaging is not so tight that it cuts off circulation or causes tingling or pain past the bandage. Bandage the area between ice treatments. |
| Elevation | Elevation of the affected area decreases swelling and pain. |
| Diagnosis | Early diagnosis by an appropriately qualified health professional and correct management are the fastest route to recovery. Consult a medical professional, especially if you are worried about the injury, the pain or swelling gets worse or the pain or swelling has not gone down within 48 hours. |
 Ice helps to prevent bleeding and further swelling
Ice helps to prevent bleeding and further swelling
 Elevation decreases swelling and pain
Elevation decreases swelling and pain
Once the injury has been diagnosed, avoid any element of HARM for 72 hours.
| Heat | Can increase bleeding and swelling and worsen pain and stiffness. |
| Alcohol | Can increase bleeding and swelling as well as masking pain and the severity of the injury. |
| Running | Rest is essential. |
| Massage | Best avoided as it can increase bleeding and swelling, thereby delaying recovery. |
Concussion
Concussion must be taken extremely seriously to safeguard the short and long-term welfare of players. Although commonly caused by a blow to the head, it can come from a blow to the body where the force of the collision is transmitted up to the brain. It is not always associated with loss of consciousness.
Concussion has many different symptoms or signs and many of these can be found in the World Rugby Concussion Guidelines at https://www.world.rugby/the-game/player-welfare/medical/concussion/concussion-guidelines
Common symptoms include poor concentration, memory loss and balance difficulties. The Pocket Concussion Recognition Tool (shown below) may help with the recognition of concussion.
If an athlete has a suspected concussion, he/she should be removed from the field of play and not allowed to return.
If a concussed player continues to play, they will put themselves at risk of greater injury and they will also let the team down because they will have difficulty processing the game happening around them.
Young players are more susceptible to rare and dangerous neurological complications, including death, caused by a second impact in an already concussed or not fully recovered individual.
Anyone removed due to suspected concussion should be assessed by a health care professional. They should not be allowed to drive a motor vehicle. Return to play should follow a graduated approach as described in the World Rugby Concussion Guidelines.
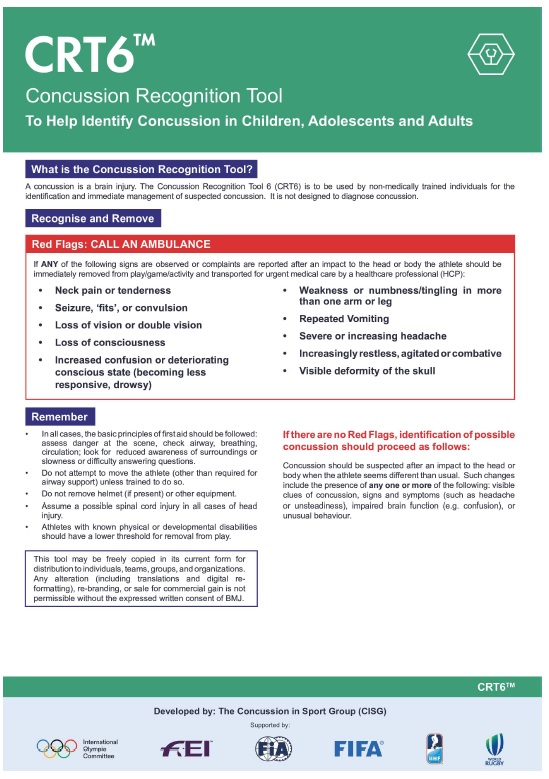
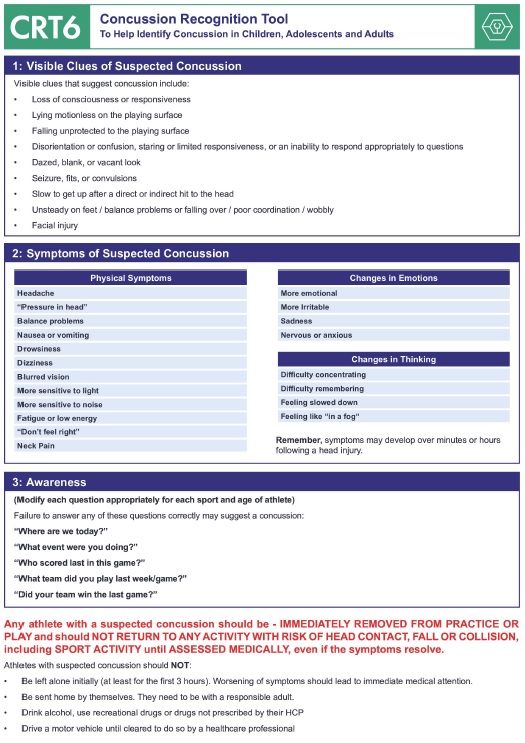
Download the Pocket Concussion Recognition Tool as an Adobe PDF file.
Rehabilitation
Rehabilitation requires supervision and management by appropriately trained medical staff, doctors, physiotherapists and fitness advisors. The aim of rehabilitation is to restore the player to full fitness, which includes:
- recovery of muscle strength
- restoration of a full range of movement in the joint
- recovery of co-ordination and balance
- fitness maintained by exercises such as cycling and swimming
- when ready - the gradual introduction of Rugby-specific skills
- contact drills followed by full contact.
Return to play
Players who return to play before full recovery place themselves at significant risk of making the injury worse or developing another injury.
Players should only return to play once the coach, doctor or physiotherapist has tested them to ensure that they are ready to get back onto the field.
These returning players must once again demonstrate that they are Rugby Ready. The tests should include similar fitness tests to those used at the beginning of the season and Rugby skills and movements that the players will perform in a game, e.g., tackling, sidestepping, jumping, etc.
Player profiling information should be used to compare performances and see if players are once again Rugby Ready. If players can demonstrate the same performance level as pre-injury, then they are once again Rugby Ready.
Normally, the best advice is, if it hurts, don’t play.
Injury reporting
Clubs should maintain a record of injuries that occur. This will enable any patterns and common injuries to be identified and appropriate preventative actions to be taken. This will also provide a record in case of any enquiries or complaints that may be made at a later date.
Where regions/provinces or Unions have injury reporting systems, it is important that these are complied with. This type of information helps inform player welfare policy and training, such as Rugby Ready.
The World Rugby Injury Report Form can be downloaded from https://passport.world.rugby/injury-prevention-and-risk-management/rugby-ready/downloads/
Disclaimer
The injury management information provided in this Rugby Ready product is intended as a tool to assist in the care and management of injured players. It does not displace the benefit of having suitably qualified personnel available to treat injuries. World Rugby (including its operating entity World Rugby Limited and other associated entities) does not accept any responsibility or liability in negligence or otherwise relation to the treatment, care or management of injured players.
Key points for players
- Ensure you are fit to play - that you are not feeling unwell, and have fully recovered from any injuries
- Ensure that you have covered any wounds
- If you have any doubt seek advice from your health care provider
Coaching tips
- Do not select players who have not fully recovered from injury
- Know what the emergency plan is
- Ensure you have and appropriate level of first aid cover for the game or training session
- Why not do a first aid course yourself?
Referee tips
Visit World Rugby’s Law Education web site
- Check who the first aider is covering the game and where they will be located
- Confirm any signals to be used
- If a player is injured and continuation of play would be dangerous, the referee must stop play
- Players must not wear any items of clothing that are contaminated by blood
- Players who have an open or bleeding wound must leave the playing area and must not return until the bleeding is controlled and the wound has been covered