Adult Basic Life Support
European Resuscitation Council Guidelines

This section is based on the European Resuscitation Council Guidelines
The above algorithm illustrates the important steps in assessing and delivering CPR to a player in cardiac arrest. Of particular importance is the early call for help, ensuring help is on its way and a call for emergency medical services (EMS)/ambulance after recognising a player is not breathing.
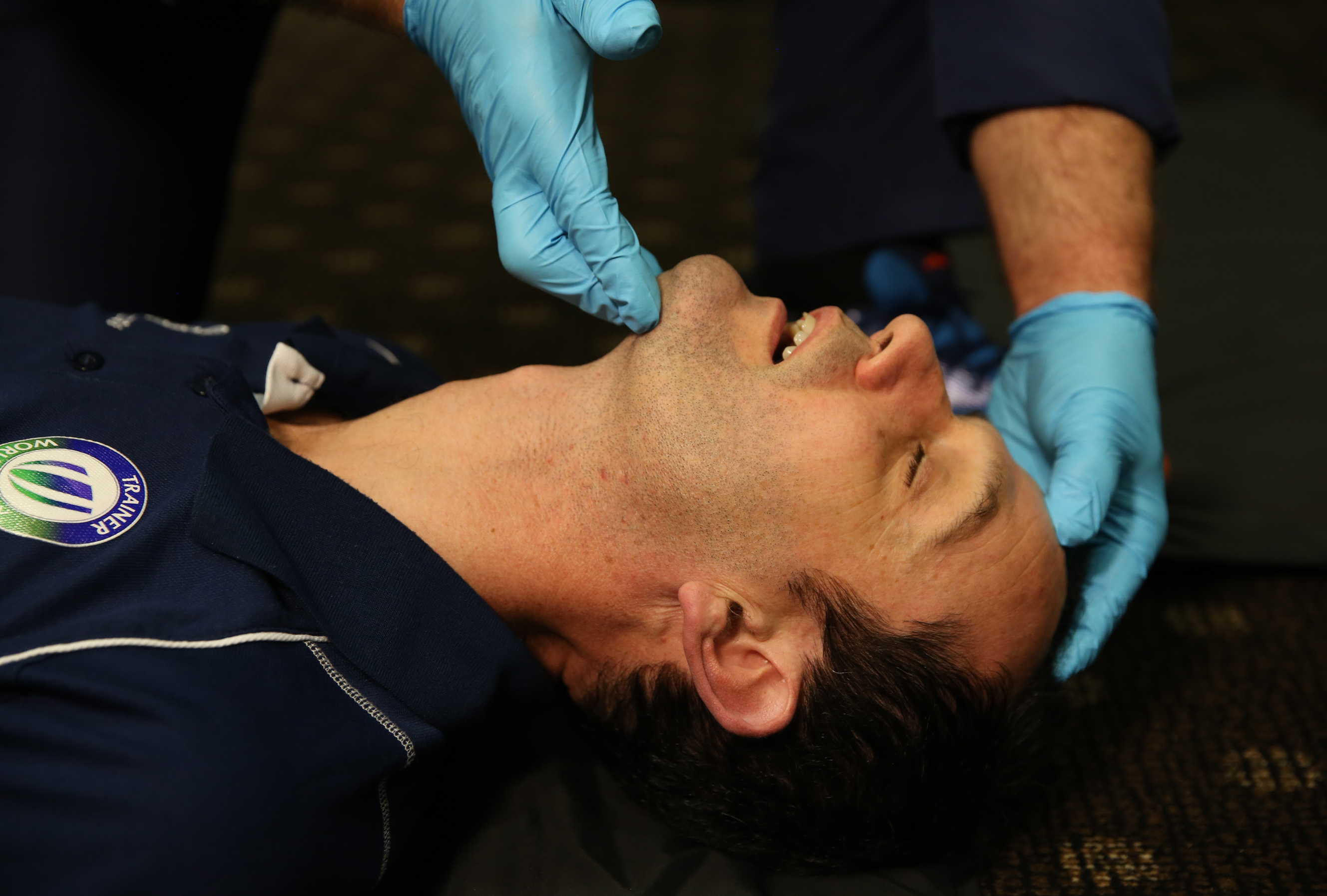
In a non-traumatic collapse, the assessment of breathing is achieved by opening the airway with a head tilt, chin lift manoeuvre and looking, listening and feeling for 10 ten seconds.
- Head tilt, Chin lift
- If cervical spine injury suspected: jaw thrust
- Look for chest movement
- Listen for breath sounds
- Feel for expired air
- Assess for 10 seconds
When a healthcare professional is in attendance, a combined airway and pulse check can be performed. This allows for the identification of a respiratory only arrest, where a pulse is present. In this scenario ventilations should be administered to the patient using a pocket mask or bag valve mask at a rate of 10–12 per minute, ensuring regular pulse checks are performed at least every minute.
If on assessing the patient there are no breath sounds and no pulse, then chest compressions should be commenced immediately, after ensuring emergency aid is on the way.

Chest compressions should be delivered in the centre of the chest, at a depth of 5-6 cm in adults and at a rate of 100 – 120 per minute. After 30 chest compressions, 2 ventilations should be delivered. These are delivered using the following steps:
- Blow steadily (1 sec) into pocket mask or use a bag valve mask.
- Allow chest to fall (1 sec)
- Repeat breath/ventilation in (1 sec)
- Allow chest to fall (1 sec)
- Total for two breathes is 4 -5 secs
- Minimal interruption to CPR
- Watch for the chest to rise
- Maintain the chin lift / jaw thrust
- Watch the chest fall

The key to this is ensuring the patient’s airway is open to deliver the breaths/ventilations and ensure no longer than 4-5 seconds are spent delivering the ventilation in order to reduce the interruption to chest compressions, maintaining coronary artery perfusion pressure.
Thereafter 30 compressions should be delivered before each 2 breaths/ventilations are delivered.
If there is a reluctance to perform mouth-to-mouth/mouth to mask/bag valve mask ventilation, then chest compressions alone are better than no CPR.
CPR should be continued until help arrives and someone takes over, the victim starts breathing adequately for themselves or the rescuers become exhausted.
American Heart Association Guidelines

Publication Name — Circulation.2020;142:S366-S468
2020 American Heart Association Guidelines for CPR & ECC – Part 3: Adult Basic and Advanced Life Support
Specifically: Page S373, Figure 2. Adult BLS algorithm for Healthcare Providers
Reprinted with permission, Circulation.2020;142:S366-S468, ©2020 American Heart Association, Inc.
https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/algorithms#adult
This section is based on the American Heart Association guidelines
Recognising cardiac arrest can be difficult. The mechanism of an unwitnessed collapse or a collapse that occurred away from contact – players do not “faint” on the Rugby pitch - should always be assessed with cardiac arrest in mind. All such casualties should be initially approached via the SABCDE and MILS system. When assessing responsiveness, tap their shoulder and shout, “Are you OK?”. Note if the player is not breathing or not breathing normally (gasping) and decide if the player needs to be moved.
To decide if a cardiac arrest has occurred in an unresponsive player, the key assessment is whether the player is breathing “NORMALLY”. This needs to be interpreted in context as the player may have been sprinting the length of the pitch just before the collapse and so you would expect them to be breathing rapidly and with symmetrical chest movement.
Safe approach: Make sure the area is clear
Assess: Tap and shout, “Are you OK?"
Call for help
Airway and breathing: Check for signs of ‘normal’ breathing; dusky colour and agonal breathing (gasping) is NOT normal
Send someone to phone for Emergency Services and bring an AED
Start CPR
Australian and New Zealand Committee on Resuscitation (ANZCOR) Guidelines

This section is based on the ANZCOR Basic Life Support Guidelines.
Recognising cardiac arrest can be difficult. The mechanism of an unwitnessed collapse or a collapse that occurred away from contact – players do not “faint” on the Rugby pitch - should always be assessed with cardiac arrest in mind. All such casualties should be initially approached once safe to do so via the DR ABCDE and MILS system. When assessing responsiveness, tap their shoulder and shout, “Are you OK?”.
If no response shout for help, once arrived send them to call for an ambulance and bring an AED.
To decide if a cardiac arrest has occurred in an unresponsive player, the key assessment is whether the player is breathing “NORMALLY”. This needs to be interpreted in context as the player may have been sprinting the length of the pitch just before the collapse and so you would expect them to be breathing rapidly and with symmetrical chest movement.
Safe approach: Make sure the area is clear
Assess: Tap and shout, “Are you OK?"
Call for help and send for help.
Airway and breathing: Check for signs of ‘normal’ breathing; dusky colour and agonal breathing (gasping) is NOT normal
Send someone to phone for Emergency Services and bring an AED
Start CPR
Attach the defibrillator and follow the instructions.