Tension Pneumothorax
Following a chest wall injury, puncture of the pleura can lead to air entering the pleural space. If a one-way valve mechanism develops, air can enter the pleural space but cannot leave at the same rate. Then with each breath, the pneumothorax will increase in size and pressure. This pneumothorax will begin to “tension” within a short space of time. This will have the effect of collapsing the ipsilateral (same side) lung, and more importantly will cause the mediastinum to shift to the contralateral (opposite) side. This has the effect of compressing or kinking the superior and inferior vena cava, drastically reducing venous return. If this is not treated rapidly, the player’s condition is likely to deteriorate into a cardiac arrest, prompt diagnosis and treatment is imperative.
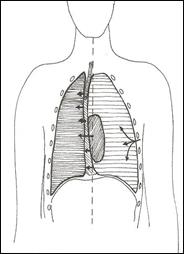
Pictorial representations of a Tension Pneumothorax
Recognition of a tension pneumothorax
- Marked respiratory distress
- Distended neck veins
- Ipsilateral reduced air entry
- Ipsilateral hyper-resonant percussion note
- Ipsilateral reduced chest expansion
- Tachycardia
- Cyanosis (late sign)
- Trachea deviated away from affected side (very late sign)
There is often concern regarding how to differentiate between a simple pneumothorax and a tension pneumothorax. There are no fixed physiological parameters which can be used, but the reality is that a patient with a tension pneumothorax is obviously compromised, in significant distress, and visibly deteriorating.
Management of a Tension Pneumothorax
- Apply high flow oxygen via a non-rebreathe mask
- Immediate decompression with needle thoracocentesis:
- 2nd intercostal space, mid clavicular line, just above third rib or
- 5th intercostal space, anterior to mid axillary line (See appendix one at the end of the chapter)
- Reassess effect of needle decompression
- Other ABCDE resuscitation as required
- Transfer to an Emergency Department as soon as possible.
Needle thoracocentesis is a temporising measure only, and the cannula can easily become kinked or occluded, which will result in the pneumothorax “re-tensioning”. For this reason, it is important that the player’s condition is continuously and closely monitored. A repeat needle decompression may be required should the first or subsequent cannula become ineffective.
More definitive subsequent interventions are thoracostomy with or without a chest seal, but should only be performed by those already skilled in these techniques, instruction in these procedures is outside the scope of this course.