Orbit
The orbit is subdivided into:
- Orbital frame - thick bony structure including the orbital rim and the zygomatic arch
- Orbital walls - thin walls which form an open pyramid, with the apex posteriorly
Orbital Floor Fractures
The orbital walls are thin and susceptible to fractures from direct pressure to the globe. It is therefore important to assess for signs of orbital wall fracture.
Inferior Orbital Wall Fracture

Signs of inferior orbital wall fracture include:
- Peri-orbital ecchymosis/bruising – lids or around the orbital frame
- Subconjunctival haemorrhage – bleeding over the sclera – suspect a base of skull fracture or a direct blow to the eye
- Lowering of the level of the pupil
- Enophthalmos
- Diplopia and reduced eye movements
N.B. children may have an inferior orbital wall fracture without any peri-orbital bruising or any subconjunctival heamorrage, known as “white eye syndrome”, making checking eye movements particularly upward gaze even more important, if missed this can lead to blindness in the affected eye.
Diplopia can be transient or persistent:
Transient diplopia
Effusion of blood into and around the extra-ocular muscles interferes with the action required to maintain co-ordination of eye movements - more evident on upward or downward gaze and may be present for several days after injury.
Persistent diplopia:
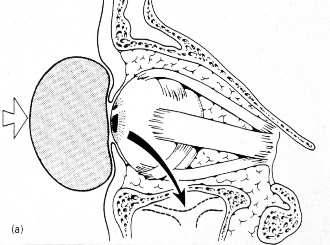
Persistent limitation of movement in a particular direction may become apparent, and this is likely to be due to interference with the action of the extra-ocular muscles. The most common cause of this is tethering of the inferior rectus muscle in the fractured floor of the inferior orbital wall.


Patients with diplopia and a suspected orbital wall fracture need referral to a maxillofacial unit for investigation and management or to an appropriate Emergency Department.
Medial Orbital Wall Fracture
Signs of medial orbital wall fracture include:
- Epistaxis
- Surgical emphysema
- Enophthalmos
- Horizontal diplopia
Retrobulbar haemorrhage
In fractures around the orbit, it is important to be aware of the potential for retrobulbar haemorrhage up to five days after the injury. It is important to impress upon the player to keep in contact and if there are any concerns, they must contact the medical team or go to an Emergency Department immediately

Specific signs which must alert the practitioner to the possibility of retrobulbar haemorrhage include:
- Proptosis - the eye is pushed forwards and gentle palpation of the eye through the eyelid, reveals a tense structure not the normal soft eyeball
- Ophthalmoplegia (inability to move the eye)
- Severe pain, out of proportion to the injury
- Reduced visual acuity
If it is impossible to open the eyelids then a good way of assessing the visual acuity is to get a pen torch and shine it on top of the upper eyelid. If the patient can “see the light” then the visual acuity is crudely ok but they will need to go for formal review if the eyelids cannot be opened at the event.