Shockable cardiac arrest rhythms
Ventricular fibrillation

Ventricular fibrillation (VF) is characterised by:
- Bizarre irregular waveform
- No recognisable QRS complexes
- Random frequency and amplitude
- Uncoordinated electrical activity
Pulseless ventricular tachycardia

Pulselss ventricular tachycardia can be of two main forms and is characterised by:
Monomorphic VT
- Broad complex rhythm
- Rapid rate
- Constant QRS morphology
Polymorphic VT
- Torsades de pointes
Once the AED has identified a shockable rhythm, it will advise that a shock should be delivered and inform the rescuers that the AED is charging. During this time, although current guidance suggests that CPR should be continued right up to the point when the shock is delivered, unfortunately most AEDs will not allow this and if they detect movement will stop charging. This highlights the importance of individual clinicians being familiar with their own equipment.
The newer AED models e.g. FR3+, do allow CPR while charging. When using a manual defibrillator, CPR should be maintained until the defibrillator is charged. It is essential that the operator of the AED ensures all other personnel have moved away and any oxygen source is removed before delivering the shock to the player in cardiac arrest.
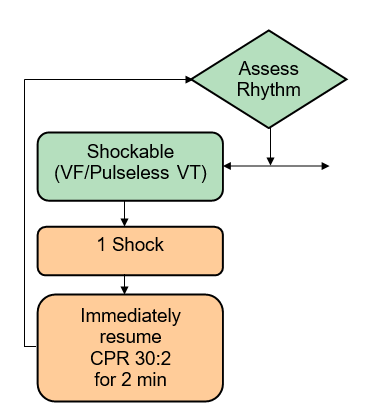
Once a shock has been delivered, CPR should be recommenced without delay. Even if defibrillation has been successful there will be a transient period of cardiac myocardial stunning, resulting in cardiac output being insufficient to perfuse the vital organs. Hence CPR should be continued for 2 minutes, after defibrillation, unless there is any sign of life.
After 2 minutes the AED will instruct the rescuers to “stand clear” whilst it analyses the heart rhythm. If the AED advises a further shock than this should be delivered and the “shockable” cycle repeated. If at any time the AED advises that a shock is not required (“no shock advised”) the rescuer should move to the “non shockable side of the algorithm.
If using a manual defibrillator, the rescuer may not receive a prompt at 2 minutes. Hence, in this situation, two minutes will usually need to be timed. A rough approximation of 2 minutes is ten breaths during a 30:2 CPR cycle. The 2 minute period of CPR should be completed with 30 compressions after the 10th breath has been delivered.
During the two minutes of CPR it is important that the reversible causes of cardiac arrest are considered. These are discussed in detail later in this chapter.
It is advised if using an AED this should be one with manual override capability. In the majority of AEDs, VT (commonest pre-arrest rhythm in adults) is only recognised for a shock if a rate of 240-250 is identified. Most elite players’ hearts will have VT at a rate of ~ 180, so having the equipment/ability to see the rhythm and manually override to deliver a shock is advised.
Medicines on the shockable side of the algorithm
If a practitioner is present who is able to gain intravenous or intra-osseous access, then medicines can be used as part of the management of cardiac arrest.
Adrenaline: On the shockable side of the algorithm, 1mg of adrenaline should be administered intravenously after the 3rd shock. This should be followed by a flush of saline. Adrenaline 1mg is then repeated every 3-5 minutes which equates to after every other shock (repeated after the 5th, 7th, 9th etc. shocks). In cardiac arrest 1:10 000 concentration of adrenaline is used, with 10 mls of 1: 10 000 being 1mg.
Amiodarone: On the shockable side of the algorithm, Amiodarone 300mg should be administered after the 3rd shock. It can be repeated in a smaller dose of 150mg after the 5th shock, but no further doses are indicated.
The recommendations suggest that adrenaline and amiodarone may be given at the same time in the cardiac arrest cycle, these should be administered and followed by at least a 20 ml flush.
For ease these drugs are best delivered using prefilled syringes.