Musculoskeletal Assessment
Primary Survey
Players with musculoskeletal injuries should be assessed and their treatment priorities established based on their injuries, vital signs and mechanism of injury. After scene safety, assessment and management should follow the ABCDE principles, as described in detail in chapter 1, ensuring life-threatening conditions are identified and treated in a timely manner.
S: Safe approach
A: Manage any airway problems and MILS of the cervical spine (if appropriate)
B: Manage any breathing problems, including adequate ventilation.
C: Circulation and haemorrhage control – this may be significant in limb trauma
D: Assess for any co-existing head injury and take measures to minimise secondary brain injury.
E: Manage the injured limb once the ABC's have been managed
The management of potentially life threatening injuries involving airway or breathing must always take priority over extremity fractures. The exception to this rule is in the presence of exsanguinating external haemorrhage. The recognition and management of most non- life-threatening external haemorrhage occurs during the circulatory assessment. Less obvious bleeding or limb deformity will usually be recognised during the exposure component of the primary survey or during the secondary survey.
Potentially significant blood loss and hypovolaemic shock can occur from untreated limb fractures. The estimated blood loss for a closed fracture of the femur is 1000-1500ml and these figures can be doubled in open fractures (Lee and Porter, 2005).
Control of external haemorrhage should precede fluid resuscitation and should follow a stepwise progression. Firstly, apply direct pressure using sterile dressings and elevation of the limb. If this does not stem the bleeding, then the wound should be packed with a dressing. A simple but important technique in reducing haemorrhage is the application of traction to realign the limb. Following a neurovascular assessment, realignment and splinting can be used to stabilise the fracture, followed by a neurovascular re-assessment.
Secondary Survey
During the primary survey, life and limb-threatening conditions should be identified and management commenced immediately. A secondary survey should only be carried out after the primary survey and any necessary resuscitation has been completed, and the patient’s condition is improving. Examination for musculoskeletal injuries should follow the “look, feel and move” principles of assessment, as well as considering the mechanism of injury. The following are signs and symptoms of a lower limb fracture or dislocation:
- anatomical deformity
- pain
- external haemorrhage
- swelling
- tenderness on palpation
- crepitus
- neurovascular compromise
Once a fracture or dislocation has been recognised it should be managed appropriately. During the rapid primary survey any signs of shock must be managed during the circulation assessment, this may involve haemorrhage control and fluid resuscitation. The on-field management of a lower limb fracture or dislocation should consist of identifying any deformity of the lower limb that requires manipulation to allow the limb to be splinted. The neurovascular status must be assessed before and after any intervention, including re-alignment. Neurovascular compromise with limb deformity requires immediate realignment after the administration of adequate analgesia. The limb can normally be realigned by applying longitudinal traction with proximal counter-traction and manual correction to a neutral position. Repeated neurovascular assessment should continue post-reduction. If there is still neurovascular compromise, the limb should be splinted and the player taken immediately to an ED for definitive care. In the event of deterioration in neurovascular status following alignment, the limb should be returned to, and splinted in, the original position and transferred to ED as a matter of urgency. Any open fractures should be covered with saline-soaked sterile dressings and prophylactic IV antibiotics considered if there is likely to be a prolonged transfer time to the Emergency Department.
An algorithm for the pre-hospital management of lower limb fractures (Lee and Porter 2005) is shown in figure 1.
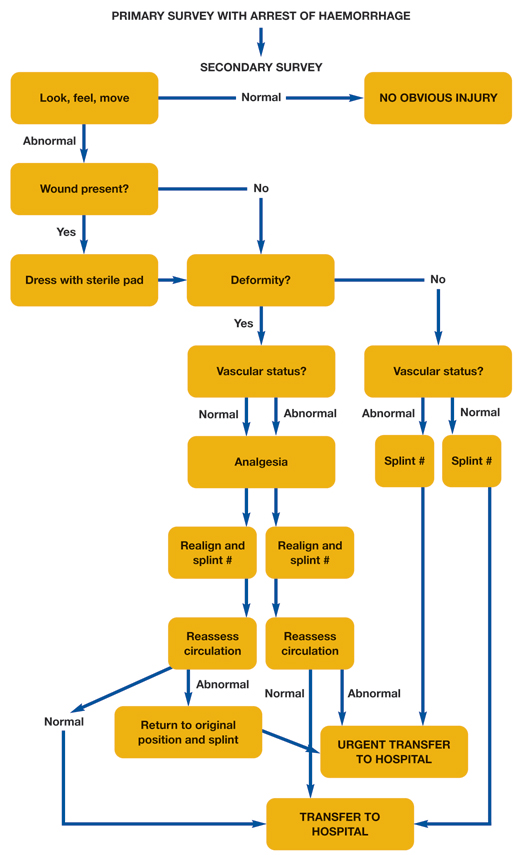
Figure 1: Algorithm for the pre-hospital management of lower limb fractures (Lee, C. and Porter, K. 2005)