Non-Shockable cardiac arrest rhythms
Asystole
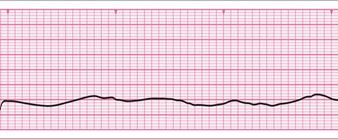
Asystole is characterised by:
- Absent ventricular (QRS) activity
- Atrial activity (P waves) may persist
- Rarely a straight line trace
Pulseless Electrical activity
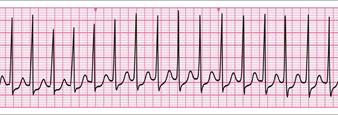

- Clinical features of cardiac arrest
- Normal looking ECG but without an output
When the AED identifies a non-shock able rhythm it will state “no shock advised” and will suggest starting CPR. In the player in cardiac arrest, CPR should be commenced immediately starting with chest compressions for 2 minutes. After 2 minutes the AED will ask the rescuers to stand clear while analysing the heart rhythm. If there is still “no shock advised” the rescuer should perform CPR for a further 2 minutes and the cycle will repeat. If the AED advises a shock this should be delivered, and the “shockable” cycle followed.
If using a manual defibrillator, the rescuer will not receive a prompt at 2 minutes, in this situation, two minutes will need to be timed. A rough approximation to 2 minutes is ten breaths/ventilations during a 30:2 CPR cycle. The 2 minute period should be completed with 30 compressions after the 10th breath has been delivered.
During the two minutes of CPR, it is important that the reversible causes of cardiac arrest are considered. These are discussed in detail later in this chapter.
Drugs on the non-shockable side of the algorithm
If a practitioner is present who can gain intravenous or intra-osseous access, then drugs can be used as part of the management of cardiac arrest.
Adrenaline: On the non-shockable side of the algorithm 1mg of adrenaline should be administered as soon as IV or IO access is established, followed by a flush. Adrenaline 1mg is then repeated every 3-5 minutes which equates to every alternate cycle
In cardiac arrest a 1:10 000 concentration of adrenaline is used (10 ml of 1:10,000 is 1 mg).
The non-shockable algorithm is summarised in the below diagram:
Reversible causes of Cardiac arrest: “The 4H’s & 4T’s”
While CPR is ongoing for the patient in cardiac arrest it is imperative that the rescuers try to ascertain the cause of the arrest so that it may be corrected if possible. The reversible causes for the arrest are known as the 4H’s & 4T’s:
- Hypoxia
- Hypovolaemia
- Hypo/hyperkalaemia & Metabolic disorders
- Hypothermia
- Tension pneumothorax
- Cardiac tamponade
- Toxins
- Thrombosis
In the pre-hospital setting it will not be possible to treat, or even accurately diagnose all of these conditions. However, the following should be given particular consideration.
Hypoxia: can be minimised by delivering high flow oxygen via a patent airway.
Hypovolaemia: must be addressed by controlling haemorrhage and administering IV/IO fluids as per guidelines.
Hypothermia: is addressed by keeping the patient covered from the elements. Cardiac arrest due to hypothermia has particular considerations. See the medical emergencies chapter for more details.
Tension pneumothorax: If suspected this should be decompressed by needle thoracocentesis.
There is little that can be done for the other causes in the pre-hospital setting. The patient in cardiac arrest should be transferred to a medical facility once safe to do so. The effectiveness of CPR in a moving ambulance is low unless there is specific equipment for this.
During the treatment of an patient in cardiac arrest, if there are any signs of life, then an ABC check of the player should be undertaken to check if there has been a return of spontaneous circulation.